Abstract
Introduction
Monoclonal gammopathy of undetermined significance (MGUS) is a prevalent hematological condition among elderly population with incidence rates of 3% and 5% over the age of 50 and 70 years, respectively (Kyle et al., 2018). It is considered a premalignant state of multiple myeloma with a risk of progression of 1% per year. It has also been shown that MGUS patients have a shorter survival compared to the age- and sex-matched cohort (Kyle et al., 2018).
Recent reports have highlighted the clinical significance of monoclonal gammopathy and the organ injury that may result from the effects of paraproteinemia (Fermand et al., 2018). With new insights into the significance of monoclonal gammopathy, the purpose of our study was to characterize the MGUS patient population referred at our hematology clinics by observing the reason for monoclonal protein testing and assessing patient comorbidities at the time of MGUS diagnosis.
Methods
We collaborated with three different clinicians who see the majority of MGUS patients at the University of Calgary Medical Group (UCMG) clinics. Patients who were referred and diagnosed with MGUS at the hematology clinic at UCMG since 2014 were assessed. Retrospective chart reviews were performed and reasons for monoclonal testing were recorded as indicated in referral request notes or initial consult notes. Data on patient comorbidities was collected as indicated in the initial consult notes. MGUS risk stratification was calculated per previous reports (Katzmann et al., 2013; Kyle et al., 2018)
Results
A total of 606 MGUS patients were seen at our clinic from February 2014 to June 2018. There were 565 patient charts available for complete review. 56% of the patients were male. Median age was 72 and median follow up was 2 years. MGUS risk stratification showed that 33.2% had low, 47.9% intermediate-low, 17.8% intermediate-high, and 1.2% high-risk MGUS. There were 55.5% IgG-MGUS, 20.5% IgM-MGUS, 12.3% IgA-MGUS, and 8.4% light chain-MGUS patients. 3% had biclonal gammopathy.
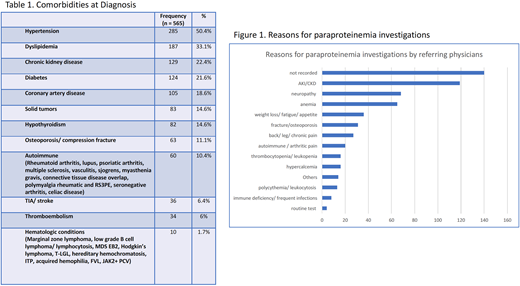
Patient comorbidities at time of diagnosis are reported in table 1. The most common conditions were hypertension (50.4%), dyslipidemia (33.1%), chronic kidney disease (22.4%), diabetes (21.6%), coronary artery disease (18.6%), and solid tumors (14.6%). The most common solid tumors were prostate cancer (22/ 83, 25%), colon cancer (12/83, 14.4%), and breast cancer (10/83, 12.0%).
Of the 565 patient charts, 140 had either missing referral sheets or had no record of the reasons for paraproteinemia investigations in the notes. In the rest of the 425 patients, the most common reason for monoclonal protein testing by referring physician was for renal dysfunction, which included work up for acute kidney injury, chronic kidney injury, proteinuria and hematuria. The next most common reason was work up of neuropathy, followed by anemia, and constitutional symptoms (figure 1). The patients in the 'Others' group had various reasons for testing including work up for seizure, forgetfulness, stroke, headache, chronic pancreatitis, multiple sclerosis, myasthenia gravis, family history of myeloma, history of venous thromboembolism, splenomegaly, bronchiectasis, chest pain, and as part of routine physical and blood donor testing.
Discussion and Conclusion
MGUS is often incidentally detected as part of a work up for other medical conditions, and our results reveal that there is a variety of reasons for which monoclonal testing is performed. With recent developments in our understanding of the significance of monoclonal gammopathy and its association with certain renal and organ damage (Fermand et al., 2018; Leung et al., 2012), there may be a change in how the paraproteinemia investigations are utilized by clinicians in different disciplines. It will be important to recognize and establish appropriate indications for testing. Furthermore, MGUS patients present with a wide range of comorbidities at the time of diagnosis. Interdisciplinary care will play a key role in discerning how much of the organ dysfunction and patients' symptoms are secondary to their underlying medical conditions versus the effect of monoclonal gammopathy.
McCulloch:Celgene: Honoraria; Takeda: Other: Travel expenses. Neri:Celgene: Consultancy, Honoraria; Janssen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal